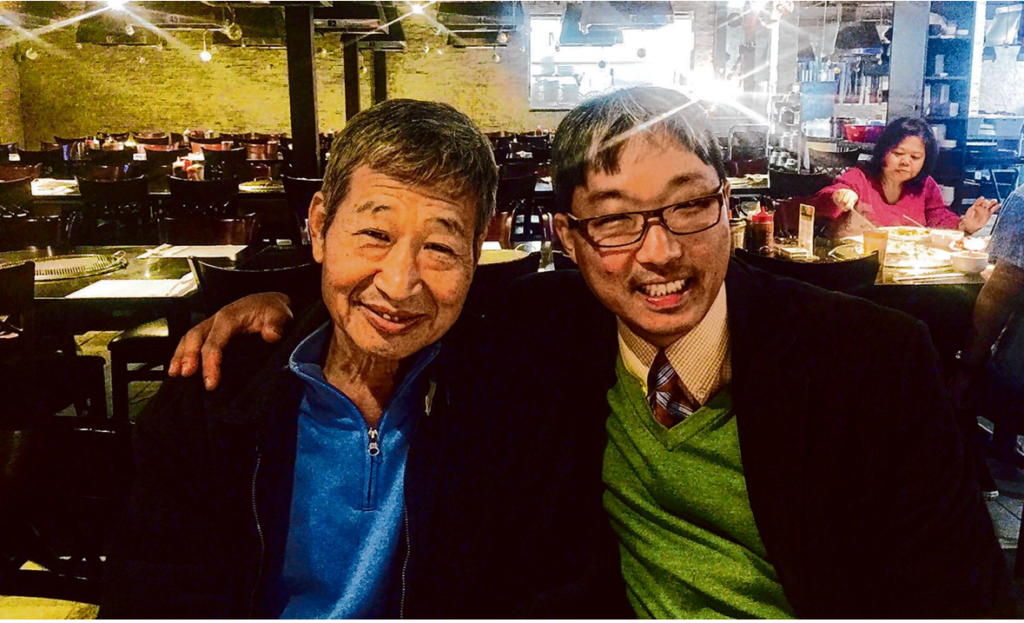
It was October 2012, and I was running amok through the city of Pittsburgh. I was down to my last day in a posh hotel room before I maxed out my only remaining credit card. After wandering the hotel halls, playing the piano outside a conference room until hotel staff shoo-ed me away, I finally went back to my room and stared at my cell phone, trying to decide whether or not to call my dealer. Then I noticed the minibar. Six years of sobriety soon went down the drain. I wasn’t some irresponsible kid partying like a rock star. I was suffering from what’s called a “dual diagnosis,” severe mental illness and substance use disorder — in my case grave bipolar disorder and an addiction to alcohol, cocaine and metham- phetamine. At some point during my Pittsburgh bender, I asked my fiancee to come see me in my room. She witnessed my erratic behavior and left to alert my father, who had recently flown in from Los Angeles. He showed
up at my hotel to confine me, alongside police in case I resisted. “Jason, no more nonsense,” he told me. “Let’s go!”
So I went, uncuffed, in a police car to a locked mental health facility where patients cannot leave without the attending psychiatrist’s permission. I was placed on a “302 hold,” which in Pennsylvania is a temporary involuntary commitment to a mental health institute for emergency psychiatric evaluation. The person who signs the 302 must have firsthand knowledge of the person and the danger they pose to themselves or others. In this case, the signature came from my father. Unlike what I would later discover back in California, a person’s family takes the lead in committing someone against their will in Pennsylvania, while society (i.e., the police) takes a back seat. Once at the facility, I was evaluated and then escorted upstairs to my private room. I desperately wanted to leave, but I was very ill. I urinated in one corner of my room to make it mine and wrote on the door: “Abandon hope all ye who enter
here.” One time, I smeared feces into a cup, covered it with my jacket, and put it on a tray outside my door. I soon heard the shrill scream of a disgusted cafeteria worker come from down the hall. When another resident of the facility called me out, I went after him, smothering his face into the carpet. “Get— off — me!” he wailed. Being unmedicated, I was prescribed lithium, a mood stabilizer and Seroquel, an anti-psychotic. Medication “compliance,” not “adherence,” was expected. Each day, patients like me waited in line outside the nurse’s station, and one by one we downed the pills from a small paper cup and then immediately drank a small paper cup of juice. We then opened our
mouths for inspection by the nurse. It was made clear to us patients: Don’t create any unnecessary hassle for the treatment
team. My psychiatrist commanded a benevolent authority. So, I complied. At my social worker’s gentle request, I attended individual,
group and men’s therapy, generating productive and healing discussions. There was camaraderie among the patients and
sincerity on the part of the staff. The other patients all had their own demons. There was the girl who liked to swallow the
plastic caps from toothpaste tubes. There was the homeless Vietnam veteran who yelled thathe deserved a medal about some
battle he was in. There was the deaf young man who had trouble keeping his hands off the nurse who checked blood pres-
sure in the morning. There was the young man who desperately wanted to leave because his girlfriend was pregnant, but the
staff said he was still too sick to go. Over time, medication and therapy worked to soothe my troubled psyche, and the facility’s environment encouraged recovery. I had my own room with a comfy bed and a view of the sky. The hall walls were a
cheerful yellow. The carpeted floors were warm. I performed Scott Joplin’s “Maple Leaf Rag” on a piano for everybody. My
fiancee, mother and school classmate stopped by. Meals came three times a day, on time. They were good enough to have seconds, which we were granted if we asked. We watched the Steelers beat the Ravens on a flat-screen TV. My fervent desire to drink
and use drugs abated slowly as I became stronger psychologically, due to good therapeutic work and being sequestered from the
temptations of the outside world. One day it dawned on me: This place had excellent doctors and staff as well as a healing setting that met my basic needs. I wanted to stay! But after 50 days, I was pushed out of the nest and put on a plane for my hometown, Los Angeles. Back home, I received a phone call: The entire charge for my mental hospital stay would be forgiven. I started crying after I heard that because I had no money and was almost positive that they were going to lower the boom on me. I returned to seeing my old
psychiatrist in Los Angeles, who didn’t bother to change my medication regimen. She did nothing but talk. I also began with a new
psychologist, who hardly talked at all. This whole time I was without insurance, so my parents paid for my uninspired
treatment out of pocket. Perhaps unsurprisingly, a year later, my troubles returned. The lack of therapeutic support and inadequate medication induced a mania. The corner liquor store soon became a tempting target. Sobriety once again receded from view. This time, my family requested a “5150,” which in California allows a peace officer or clinician to confine someone against their will temporarily for mental health assessment. The person must be homicidal, suicidal or “gravely disabled.” I had sent threatening emails to my family.
The police came to my apartment, handcuffed me and hauled me into a cell for observation. Later, I was assigned housing and appointed a “conservator” by a court to manage my finances and daily affairs. In contrast to my 302 in Pittsburgh, police and the conservatorship system took the lead in assessing mental health. My family had to follow behind.
My relationship with the person overseeing my conserva- torship was rocky and I chafed under his discipline. He insisted
on an intensive outpatient program. For a while, I hung in there. But after a month I broke down. After being sequestered in an emergency room, I threw a bread roll at my conservator when he showed up. “Catch it! Pick it up! Eat it!” I yelled. “Stop, Jason, or else!” he responded. I chose “or else.” My temper and erratic behavior continued. I was strapped to a gurney, elevated into an ambulance and taken to a locked facility. I had no money and no insurance. My family was tired of paying my medical bills, and I don’t blame them. The psychiatrist put me back on lithium, as before, and Risperdal, another antipsychotic. The facility was bleak. Though therapy was mandatory, the therapists were just going through the motions. I shared a room with two other people. Sleep-deprived from their noise, I became delirious. The hall walls were painted a repulsive government green. The linoleum floor froze my feet. The fluorescent lighting cast a moonlike pall. There was no piano here. I couldn’t digest the food. I began vomiting uncontrollably and lost 25 pounds in 17 days. There was no hope for recovery. We patients were zombies.
Finally, I begged staff to let me see my parents. They appeared hours later. A new psychiatrist,
one they found on their own, assessed me that evening. The next morning, a nurse announced my discharge: “Jason Park! You’re going to … Malibu?” Only with my parents’ intervention and resources did I get the help I needed at a private facility. Thanks to the high level of care I received, I was eventually able to live a normal life and became a college professor and
now an author. For the thousands of homeless people with dual diagnoses in California, it’s safe to say the pathway to a similar recovery is much slimmer. It doesn’t have to be. As California weighs meaningful changes to its conservatorship system, and Gov. Gavin Newsom announces plans to
build thousands of new mental health beds in the state, I believe my experiences in Pennsylvania
and California offer lessons for how we can and should move forward.
To begin with, many of our facilities, like the one my conservator placed me in Los Angeles, are not healing environments capable of assisting people in getting their lives back on track. They are traumatizing. When you hear stories of routine violence at state mental health centers, the horrible conditions no doubt play a role. But patients could stand to benefit from more subtle changes, too.
Unlike in Pennsylvania, where my family made the tough call to commit me against
my will, here in California it is public authorities, most often beginning with the police, who
make the decisions. A court appoints a conservator to take care of the conservatee’s finances and daily affairs. My father wanted to be my conservator, but the court decided that it
would be in my best interests to appoint its own. Family and society are pitted against each other, both fighting for control, instead of working smoothly together, hand in hand.
To rectify this, everyone should have the option of a family co-conservator alongside a
co-conservator appointed by society. As the conservatee re-covers and wants greater control of their finances or daily affairs, he or she must secure the approval of one of these co-conservators — an inexpensive and caring system of checks and
balances. Not all people struggling with mental health and substance use issues have families as patient, loving and supportive as mine. But many do. Empowering them to play greater roles worked for me in Pittsburgh. It could work for others here in California, too.

Keeping guns from falling in the wrong hands — lessons from Charlotte
On April 30, four police officers were killed in a shooting while attempting to serve a warrant at a home in Charlotte, N.C. Four other